 June
20
June
20
Tags
When Illusions Help
What can pushing the limits of reality do for you? There has been a lot of interest recently in using the mind-altering properties of a class of drugs known as psychedelics in the treatment of many psychiatric and neurological disorders. Currently, psychedelics are being explored as a novel treatment for depression, anxiety, post-traumatic stress disorder, obsessive-compulsive disorder (OCD), and more recently, seizure disorders. Psychedelic-assisted treatment (PAT) has been shown to be an efficacious treatment option for all of these conditions. However, according to Canadian researchers Freidel et al. (1), a cohort of patients has been overlooked in past research: those with epilepsy and a variety of other seizure disorders.
Epilepsy affects an estimated 50 million people worldwide (2), and it can increase their risk of mortality and morbidity, impact their ability to find and hold a job, and even affect their quality of life. Additionally, the number of people affected by non-epileptic seizure disorders is roughly estimated to be anywhere from tens of millions to even hundreds of millions. Given these staggering numbers, as well as the fact that many people with seizure disorders are treatable with the current treatments (3), it is very curious that these patients have been left out of the research on PAT. However, by looking at the limited research specifically determining the safety of PAT for patients with seizure disorders, as well as the pharmacology of psychedelics themselves, we may begin to understand why this is the case.
Psychedelics, Historically
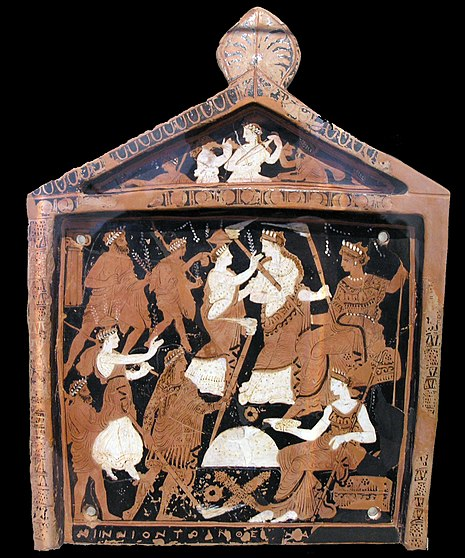
There are many historical accounts of ritualistic hallucinogen use, starting before the common era (BCE) with the ancient Greeks. One famous example of this is their ingestion of a psychoactive drink in seasonal religious rites known as kykeon; this drink is thought to have LSD-like psychedelic substances (4). These rites, known as the Eleusinian Mysteries, were secretive ceremonies where the ingestion of kykeon was believed to bestow “revelatory mind states with profound spiritual and intellectual ramifications” on the participants of this ceremony (5).
This is just one example, but there are countless other historical accounts of the use of psychedelics for various purposes, across cultures around the world, and throughout the ages. However, beginning in the 1960s, the prohibition of psychedelics by the United States and the United Nations has stifled cultural and medicinal usage, as well as scientific research, of these substances (4). Recently, research into how they could be efficacious for the treatment of many psychiatric and neurological disorders has been gaining traction again. Before we get into their clinical applications, let us take a look at what we currently know about how these illusory compounds work.
Psychedelics: What are They?
Psychedelics are a subclass of hallucinogens–a large class of psychoactive drugs that can cause major alterations in thought, mood, and perception. Psychedelics, then, are defined as “hallucinogenic drugs whose primary effect is to trigger non-ordinary mental states (known as psychedelic experiences or “trips”) and an apparent expansion of consciousness” (6). The exact neural mechanisms of psychedelics are still under debate, but there is a general consensus that most psychedelics interact with the neurotransmitter serotonin to some degree (7;8).
Neurotransmitters are the brain’s chemical messengers and are responsible for most if not all of the brain’s functions. One of serotonin’s most important roles in the brain is the regulation of mood, and because psychedelics increase serotonin release, they contribute to mood elevation, positive outlook, and increased desire for social interaction, and thus may explain serotonin’s antidepressant effects in the brain (9). Additionally, serotonin also creates hallucinations when in excess, which may in part because its receptors increase dopamine activity, the “feel good” neurotransmitter that rewards you and induces euphoria. Furthermore, when in large amounts, dopamine causes hallucinations (schizophrenia, a disorder which is primarily believed to be caused by dopamine dysregulation, has symptoms of delusions and hallucinations; 10, 11) Now that we know how psychedelics affect the brain, what actually distinguishes the two classes?
Psychedelics themselves can then be divided into two classes, based on the supposed neural mechanisms that elicit these effects: classical psychedelics and atypical psychedelics. Classical psychedelics are known to activate serotonin receptors directly (called agonism), and are thus able to produce vivid visual and auditory hallucinations at higher doses. Two classical psychedelics, psilocybin (“magic mushrooms”; 12) and lysergic acid diethylamide (LSD or “acid”; 13), are in fact high-affinity serotonin agonists, with LSD having the greater effect on serotonin receptors and thus producing more vivid hallucinations. Atypical psychedelics, on the other hand, still produce some serotonin agonism, but to a lesser extent than classical psychedelics and also interact with a wider variety of neurotransmitter receptors,and are mostly known for manifestations other than hallucinations. Two atypical psychedelics, methylenedioxymethamphetamine (MDMA, “ecstasy”, “E”, or “molly”; 14) and ketamine (“K”; 15, 16), are such examples. MDMA is primarily known as a stimulant (a substance that makes one feel energized), whereas ketamine is actually used in medicine as an anesthetic. MDMA affects serotonin to a lesser extent (and in different ways), but it also directly stimulates dopamine receptors, another neurotransmitter that causes hallucinations. Ketamine, on the other hand, has a completely different primary effect in the brain: ketamine inhibits the release of the brain’s main excitatory neurotransmitter, glutamate. This is responsible for ketamine’s primary antidepressant and anticonvulsant effects, and this reduction of glutamate is what makes it an excellent general anesthetic at higher doses.
.
Epilepsy at a Glance
Epilepsy is a seizure disorder that causes recurring (more than 1) seizures that are unpredictable and have no apparent cause (e.g. drug overdose, electrocution, brain trauma, etc). Furthermore, seizures are a symptom of many disorders that are a result of overexcitation in the brain, or the synchronized firing of many neurons at once.
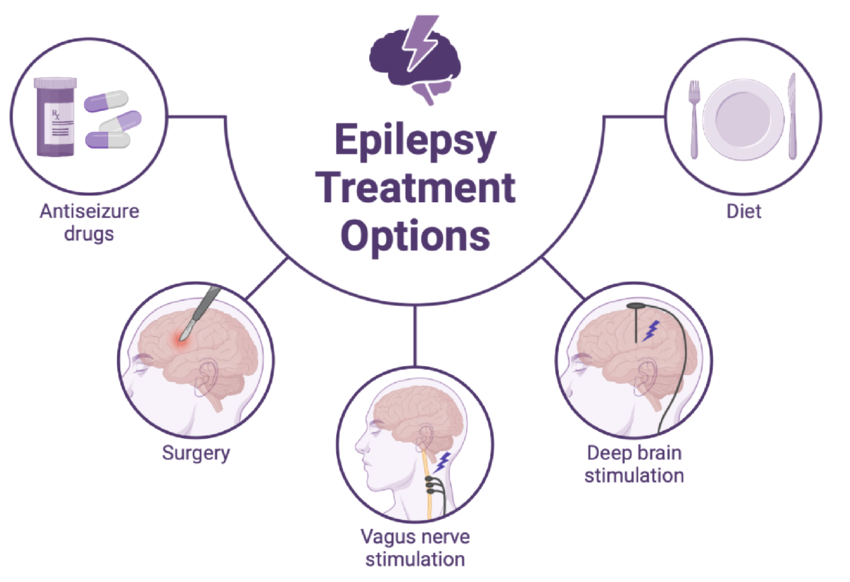
A principal cause of seizures is glutamate: when there is an imbalance in glutamate’s regulation, it becomes toxic and can have many detrimental effects on the brain, such as causing overexcitation. Because of this, some antiepileptic drugs (AEDs) target the brain’s glutamate receptors–i.e. inhibit them–to try to lower the concentration of glutamate in the brain. Ketamine functions in a very similar manner, and this may contribute to ketamine’s antiepileptic properties. There are many AEDs, with various mechanisms to treat epilepsy, but a lot of them can have side effects, and some types of epilepsy/seizure disorders are not even controlled by AEDs. In recent years, devices that are implanted in the body or brain have been developed as another treatment option to help control seizure frequency or disrupt seizure onset, but these also have their drawbacks (risks and complications of surgery, side effects of the device itself, limitations, etc.). Therefore, there is a real need for alternative treatment methods for those with epilepsy and seizure disorders. This is where the potential safety of PAT comes in.
Since most of the cases that will be described actually talk about patients experiencing seizures after taking psychedelics, it may seem dangerous to recommend taking this class of drugs to those who are already susceptible to seizures. However, what if there were other factors in these cases that show us that psychedelics taken in monitored conditions are safe and even beneficial for those with seizure disorders?
Case Studies
Research from 2022 (17) suggests that increases in serotonin levels increase excitation in the brain, and this extrapolates that inhibition of these serotonin receptors would produce anti-convulsant effects. Since all the psychedelics mentioned interact with serotonin receptors (excite) to some degree, you may begin to wonder how that makes them a viable candidate for the safe treatment of seizure disorders. In fact, it is true that many case studies in the field mention patients experiencing seizures. However, in all of the cases where seizures were provoked, there were either high doses (psilocybin; 18), unknown/unspecified doses (due to either accidental or recreational ingestion; 19-24), and/or concurrent drug use (most often alcohol, a drug known to increase seizure likelihood; 1,25,26). Thus, all of these could be contributing factors to the results and render them uninformative for our purposes.
On the other hand, in those who took lower doses/doses in clinical settings, seizure frequency either stayed the same (27,28) or was reduced (27,16). In comparison to the aforementioned studies, it seems that these controlled variables are crucial for the treatment’s success/efficacy. In the case of PAT with ketamine, there was a complete remission from seizures during treatment, most likely due to inhibition of glutamate being the primary mechanism of action. Similarly, treatment with LSD in a clinical setting primarily showed no difference in seizure frequency compared to baseline, and psilocybin at a low dosage as well, suggesting that low levels of serotonin increase do not exacerbate seizure disorders or increase seizure frequency. Although this data set is small, it is important to emphasize that the cases from clinical settings with monitored doses proved efficacious for treatment or did not increase seizure risk. This data combined with what we understand to be the neural mechanisms of each of the discussed drugs, it seems we may start to see more research that investigates epilepsy eligibility for PAT.
Conclusion
As we venture into the realm of psychedelic-assisted treatment (PAT) for psychiatric and neurological conditions, the oversight of individuals grappling with epilepsy and seizure disorders is unmistakable. Despite the historical and pharmacological evidence hinting at psychedelics’ potential as anticonvulsants, reservations persist regarding their safety within this particular population. However, a nuanced analysis reveals promising outcomes within controlled settings, underscoring the need for further investigation to unlock PAT’s therapeutic potential for managing seizures. In navigating this uncharted territory, rigorous inquiry emerges as the guiding force, illuminating pathways toward transformative treatment options for those struggling with epilepsy and seizure disorders.
REFERENCES
- https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2023.1326815/full
- https://www.who.int/news-room/fact-sheets/detail/epilepsy#:~:text=Rates%20of%20disease,as%20139%20per%20100%20000.
- https://www.uptodate.com/contents/evaluation-and-management-of-drug-resistant-epilepsy#:~:text=As%20many%20as%2020%20to,likely%20to%20have%20refractory%20epilepsy.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8412860/
- https://en.wikipedia.org/wiki/Eleusinian_Mysteries#Entheogenic_theories
- https://en.wikipedia.org/wiki/Psychedelic_drug#:~:text=While%20the%20term%20psychedelic%20is,sativa%2C%20Nymphaea%20nouchali%20and%20Salvia
- https://www.sciencedirect.com/topics/neuroscience/serotonergic-psychedelic
- https://www.nature.com/articles/1395318
- https://onlinelibrary.wiley.com/doi/full/10.1111/j.1755-5949.2010.00135.x
- https://www.psychiatry.org/patients-families/schizophrenia/what-is-schizophrenia#:~:text=Schizophrenia%20is%20a%20chronic%20brain,thinking%20and%20lack%20of%20motivation.
- https://www.healthline.com/health/schizophrenia/schizophrenia-and-dopamine#:~:text=Increases%20in%20dopamine%20activity%20in,factors%20involved%20in%20schizophrenia%20symptoms.
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8156539/
- https://en.wikipedia.org/wiki/LSD
- https://pubmed.ncbi.nlm.nih.gov/18035407/#:~:text=In%20addition%20to%20its%20stimulatory,dopaminergic%20and%2For%20serotonergic%20receptors
- https://www.jci.org/articles/view/130808
- https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2023.1197409/full
- https://onlinelibrary.wiley.com/doi/full/10.1002/epi4.12580#:~:text=In%20vitro%20data%20show%20that,would%20induce%20anti%2Depileptic%20effects.
- https://doi.org/10.3389/fneur.2023.1214969
- https://pubmed.ncbi.nlm.nih.gov/9973755/
- https://doi.org/10.1136/emj.14.3.183
- https://www.tandfonline.com/doi/full/10.1080/15563650.2021.1999464?scroll=top&needAccess=true
- https://doi.org/10.1007/s00431-013-2080-x
- https://doi.org/10.1176/ajp.149.6.843b
- https://doi.org/10.1007/s12028-008-9096-5
- https://doi.org/10.1007/BF01709744
- https://doi.org/10.1093/jat/bkaa145
- https://link.springer.com/article/10.1007/BF00402367
- https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2023.1214969/full




You must be logged in to post a comment.